COVID-19 POSTER AND ASSIGMENT
For IT and Eglish lesson!
Do you know why we have to stay at home?
Staying at home can help stop coronavirus spreading- not go to work, school or public areas
- not use public transport or taxis
- not have visitors, such as friends and family, in your home
- not go out to buy food or collect medicine – order them by phone or online, or ask someone else to drop them off at your home
You'll need to stay at home if you have symptoms of coronavirus (COVID-19) or live with someone who does.
Staying at home means you should:
You can use your garden, if you have one. You can also leave the house to exercise – but stay at least 2 metres away from other people.
And assigment COVID-19
STUDENTS’ WORK SHEET CORONA VIRUS ( COVID-19)
THE INSTRUCTIONS :
1. Learn various information about Viruses and Corona Viruses from various sources that you can access from various media.
2. This material in this worksheet is only one alternative learning source 3. Complete the tasks given in the worksheet
4. For assignments in the form of design products, collected during the Learning Process through face-to-face re-starting to be active (the product is photographed in advance and sent via social media that you can publish in your own blog.
5. The assignment is submitted no later than March 21, 2020
INTERNATIONAL PROTOCOL TO RESPONSE COVID-19 (Sources : World Health Organization)
The Global Response & Next Steps
1. The COVID-19 virus is a new pathogen that is highly contagious, can spread quickly, and must be considered capable of causing enormous health, economic and societal impacts in any setting. It is not SARS and it is not influenza. Building scenarios and strategies only on the basis of well-known pathogens risks failing to exploit all possible measures to slow transmission of the COVID-19 virus, reduce disease and save lives.
COVID-19 is not SARS and it is not influenza. It is a new virus with its own characteristics. For example, COVID-19 transmission in children appears to be limited compared with influenza, while the clinical picture differs from SARS. Such differences, while based on limited data, may be playing a role in the apparent efficacy of rigorously 19 applied non-pharmaceutical, public health measures to interrupt chains of human-tohuman transmission in a range of settings in China. The COVID-19 virus is unique among human coronaviruses in its combination of high transmissibility, substantial fatal outcomes in some high-risk groups, and ability to cause huge societal and economic disruption. For planning purposes, it must be assumed that the global population is susceptible to this virus. As the animal origin of the COVID-19 virus is unknown at present, the risk of reintroduction into previously infected areas must be constantly considered. The novel nature, and our continuously evolving understanding, of this coronavirus demands a tremendous agility in our capacity to rapidly adapt and change our readiness and response planning as has been done continually in China. This is an extraordinary feat for a country of 1.4 billion people.
2. China’s uncompromising and rigorous use of non-pharmaceutical measures to contain transmission of the COVID-19 virus in multiple settings provides vital lessons for the global response. This rather unique and unprecedented public health response in China reversed the escalating cases in both Hubei, where there has been widespread community transmission, and in the importation provinces, where family clusters appear to have driven the outbreak.
Although the timing of the outbreak in China has been relatively similar across the country, transmission chains were established in a wide diversity of settings, from megacities in the north and south of the country, to remote communities. However, the rapid adaptation and tailoring of China’s strategy demonstrated that containment can be adapted and successfully operationalized in a wide range of settings. China’s experience strongly supports the efficacy and effectiveness of anchoring COVID19 readiness and rapid response plans in a thorough assessment of local risks and of utilizing a differentiated risk-based containment strategy to manage the outbreak in areas with no cases vs. sporadic cases vs. clusters of cases vs. community-level transmission. Such a strategy is essential for ensuring a sustainable approach while minimizing the socio-economic impact.
3. Much of the global community is not yet ready, in mindset and materially, to implement the measures that have been employed to contain COVID-19 in China. These are the only measures that are currently proven to interrupt or minimize transmission chains in humans. Fundamental to these measures is extremely proactive surveillance to immediately detect cases, very rapid diagnosis and immediate case isolation, rigorous tracking and quarantine of close contacts, and an exceptionally high degree of population understanding and acceptance of these measures.
Achieving the high quality of implementation needed to be successful with such measures requires an unusual and unprecedented speed of decision-making by top leaders, operational thoroughness by public health systems, and engagement of society. 20 Given the damage that can be caused by
uncontrolled, community-level transmission of this virus, such an approach is warranted to save lives and to gain the weeks and months needed for the testing of therapeutics and vaccine development. Furthermore, as the majority of new cases outside of China are currently occurring in high and middleincome countries, a rigorous commitment to slowing transmission in such settings with non-pharmaceutical measures is vital to achieving a second line of defense to protect low income countries that have weaker health systems and coping capacities. The time that can be gained through the full application of these measures – even if just days or weeks – can be invaluable in ultimately reducing COVID-19 illness and deaths. This is apparent in the huge increase in knowledge, approaches and even tools that has taken place in just the 7 weeks since this virus was discovered through the rapid scientific work that has been done in China.
4. The time gained by rigorously applying COVID-19 containment measures must be used more effectively to urgently enhance global readiness and rapidly develop the specific tools that are needed to ultimately stop this virus.
COVID-19 is spreading with astonishing speed; COVID-19 outbreaks in any setting have very serious consequences; and there is now strong evidence that non-pharmaceutical interventions can reduce and even interrupt transmission. Concerningly, global and national preparedness planning is often ambivalent about such interventions. However, to reduce COVID-19 illness and death, near- term readiness planning must embrace the large-scale implementation of high-quality, non-pharmaceutical public health
measures. These measures must fully incorporate immediate case detection and isolation, rigorous close contact tracing and monitoring/quarantine, and direct population/community engagement. A huge array of COVID-19 studies, scientific research projects and product R&D efforts are ongoing in China and globally. This is essential and to be encouraged and supported. However, such a large number of projects and products needs to be prioritized. Without prioritizing, this risks compromising the concentration of attention and resources and collaboration required to cut timelines by precious weeks and months. While progress has been made, the urgency of the COVID-19 situation supports an even more ruthless prioritization of research in the areas of diagnostics, therapeutics and vaccines. Similarly, there is a long list of proposed studies on the origins of COVID-19, the natural history of the disease, and the virus’s transmission dynamics. However, the urgency of responding to cases and saving lives makes it difficult for policy makers to consider and act on such comprehensive lists. This can be addressed by balancing studies with the immediate public health and clinical needs of the response. Studies can be prioritized in terms of the largest knowledge gaps that can be most rapidly addressed to have greatest immediate impact on response operations and patient management. This suggests prioritizing studies to identify risk factors for transmission in households, institutions and the community; convenience sampling for this virus in the population using existing surveillance systems; age-stratified sero-epidemiologic surveys; the analysis of clinical case series; and cluster investigations.
For countries with imported cases and/or outbreaks of COVID-19
1. Immediately activate the highest level of national Response Management protocols to ensure the all-of-government and all-of-
society approach needed to contain COVID-19 with non- pharmaceutical public health measures;
2. Prioritize active, exhaustive case finding and immediate testing and isolation, painstaking contact tracing and rigorous quarantine of close contacts;
3. Fully educate the general public on the seriousness of COVID-19 and their role in preventing its spread;
4. Immediately expand surveillance to detect COVID-19 transmission chains, by testing all patients with atypical pneumonias, conducting screening in some patients with upper respiratory illnesses and/or recent COVID-19 exposure, and adding testing for the COVID-19 virus to existing surveillance systems (e.g. systems for influenza-like- illness and SARI); and 22
5. Conduct multi-sector scenario planning and simulations for the deployment of even more stringent measures to interrupt transmission chains as needed (e.g. the suspension of large-scale gatherings and the closure of schools and workplaces).
For uninfected countries
1. Prepare to immediately activate the highest level of emergency response mechanisms to trigger the all-of-government and all-of society approach that is essential for early containment of a COVID- 19 outbreak;
2. Rapidly test national preparedness plans in light of new knowledge on the effectiveness of non-pharmaceutical measures against COVID-19; incorporate rapid detection, largescale case isolation and respiratory support capacities, and rigorous contact tracing and management in national COVID-19 readiness and response plans and capacities;
3. Immediately enhance surveillance for COVID-19 as rapid detection is crucial to containing spread; consider testing all patients with atypical pneumonia for the COVID-19 virus, and adding testing for the virus to existing influenza surveillance systems;
4. Begin now to enforce rigorous application of infection prevention and control measures in all healthcare facilities, especially in emergency departments and outpatient clinics, as this is where COVID-19 will enter the health system; and
5. Rapidly assess the general population’s understanding of COVID-19, adjust national health promotion materials and activities accordingly, and engage clinical champions to communicate with the media.
For the public
1. Recognize that COVID-19 is a new and concerning disease, but that outbreaks can managed with the right response and that the vast majority of infected people will recover;
2. Begin now to adopt and rigorously practice the most important preventive measures for COVID-19 by frequent hand washing and always covering your mouth and nose when sneezing or coughing;
3.Continually update yourself on COVID-19 and its signs and symptoms (i.e. fever and dry cough), because the strategies and response activities will constantly improve as new information on this disease is accumulating every day; and
4.
Be prepared to actively support a response to COVID-19 in a variety of ways, including the adoption of more stringent ‘social distancing’ practices and helping the high-risk elderly population. 23
For the international community
1. Recognize that true solidarity and collaboration is essential between nations to tackle the common threat that COVID-19 represents and operationalize this principle;
2. Rapidly share information as required under the International Health Regulations (IHR) including detailed information about imported cases to facilitate contact tracing and inform containment measures that span countries;
3. Recognize the rapidly changing risk profile of COVID-19 affected countries and continually monitor outbreak trends and control capacities to reassess any ‘additional health measures’ that significantly interfere with international travel and trade.
LEARNING ACTIVITIES :
1. Read the article above on :INTERNATIONAL PROTOCOL TO RESPONSE COVID-19 and understand the Corona virus is.
2. Find out for various resources about Corona Virus to comprehend what it is about.
3. Viruses have several types, in general it has characteristics, classification and diseases that can be caused specifically. Analyze virus characteristics based on:
a. Characteristics of viruses . Among a total of 72 314 case records (Box), 44 672 were classified as confirmed cases of COVID-19 (62%; diagnosis based on positive viral nucleic acid test result on throat swab samples), 16 186 as suspected cases (22%; diagnosis based on symptoms and exposures only, no test was performed because testing capacity is insufficient to meet current needs), 10 567 as clinically diagnosed cases (15%; this designation is being used in Hubei Province only; in these cases, no test was performed but diagnosis was made based on symptoms, exposures, and presence of lung imaging features consistent with coronavirus pneumonia), and 889 as asymptomatic cases (1%; diagnosis by positive viral nucleic acid test result but lacking typical symptoms including fever, dry cough, and fatigue).
b.Virus form at the end of December, public health officials from China informed the World Health Organization that they had a problem: an unknown, new virus was causing pneumonia-like illness in the city of Wuhan. They quickly determined that it was a coronavirus and that it was rapidly spreading through and outside of Wuhan.
c. Virus structure. Coronavirus virions are spherical to pleomorphic enveloped particles (Fig. 60-3). The envelope is studded with projecting glycoproteins, and surrounds a core consisting of matrix protein enclosed within which is a single strand of positive-sense RNA (Mr 6 × 106) associated with nucleoprotein. The envelope glycoproteins are responsible for attachment to the host cell and also carry the main antigenic epitopes, particularly the epitopes recognized by neutralizing antibodies. OC43 also possesses a haemagglutin.
d. How the virus cycle life is The best studied model for coronavirus replication and pathogenesis has been the group 2 murine coronavirus, mouse hepatitis virus, and much of what is known of the stages of the coronavirus life cycle has been determined in animals and in culture using this virus. Thus this discussion will focus on MHV with comparisons to SCoV and other coronaviruses. This is appropriate because bioinformatics analyses suggest that SCoV, while a distinct virus, has significant similarities in organization, putative protein functions, and replication to the group II coronaviruses, particularly within the replicase gene
e. Propagation of the virus Corona virus transmission can occur through the following things:
Droplets or liquid droplets that come from coughing and sneezing
Personal contact such as touching and shaking hands
Touching an object or surface with a virus on it, then touching the mouth, nose, or eyes before washing hands
Fecal contamination (rare)
A recent study shows the potential for airborne transmission.
When someone coughs or sneezes and releases a virus-containing fluid, it can potentially spread into the air and can directly enter other people's bodies if they are in a close position.
f. Virus Classification Virus classification e
(unranked):
Virus
Realm:
Riboviria
Phylum:
incertae sedis
Order:
Nidovirales
Family:
Coronaviridae
Subfamily:
Orthocoronavirinae
g. Diseases caused by viruses Corona virus infection or COVID-19 is caused by coronavirus, which is a group of viruses that infect the respiratory system. In most cases, coronaviruses only cause mild to moderate respiratory infections, such as flu. However, this virus can also cause severe respiratory infections, such as pneumonia, Middle-East Respiratory Syndrome (MERS), and Severe Acute Respiratory Syndrome (SARS).
It is suspected that the Corona virus was initially transmitted from animals to humans. However, it was later discovered that the Corona virus was also transmitted from human to human.
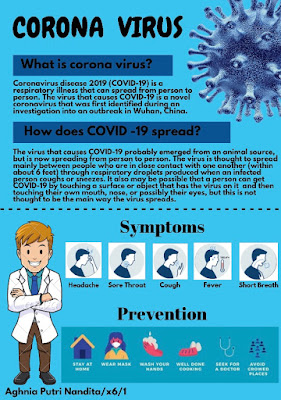
Corona virus infection or COVID-19 can cause sufferers to experience flu symptoms, such as fever, runny nose, cough, sore throat, and headache; or symptoms of severe respiratory infections, such as high fever, cough with phlegm and even bleeding, shortness of breath, and chest pain.
However, in general there are 3 general symptoms that can indicate someone is infected with the Corona virus, namely:
Fever (body temperature above 38 degrees Celsius)
Cough
Hard to breathe
4. Corona virus is a type of virus that can cause disease and it is epidemic. Evaluate based on various learning resources related to:
a. Background epidemic corona virus, Background on the Corona virus or COVID-19, the case began with pneumonia or mysterious pneumonia in December 2019. This case is thought to be related to the Huanan animal market in Wuhan which sells various types of animal meat, including those that are not commonly consumed, for example snakes, bats and various types of mice.
Cases of this mysterious pneumonia infection are indeed commonly found in the animal market. Corona virus or COVID-19 allegedly brought bats and other animals that humans eat until transmission occurs. Coronavirus is actually no stranger to the world of animal health, but only a few species are able to infect humans to become pneumonia.
Before the COVID-19 epidemic, the world had a stir with SARS and MERS, which is also associated with the Corona virus. With this background, the Corona virus is not the only time to make the world panic. Having the same flu-like symptoms, the Corona virus develops rapidly to result in more severe infections and organ failure
Bats, snakes and various other exotic animals are still considered a vector of the Corona virus or COVID-19. Regardless of whether this information is true or not, COVID-19 proves itself capable of being transmitted between people. Transmission was very rapid until the World Health Organization WHO established the Corona virus pandemic or COVID-19
b. symptoms of being infected with the corona virus, Reported illnesses have ranged from mild symptoms to severe illness and death for confirmed coronavirus disease 2019 (COVID-19) cases.
These symptoms may appear 2-14 days after exposure (based on the incubation period of MERS-CoV viruses).
Fever
Cough
Shortness of breath
c. how Corona Virus spread . The World Health Organization (WHO) revealed how to spread the corona virus from one person to another. According to WHO, when a person suffering from COVID-19 coughs or breathes, they release like drops of liquid which also contains the corona virus.
Most of the drops or liquids that fall on the surface and objects nearby, such as tables, tables, or telephones.
People can be exposed to or infected with COVID-19 by touching a contaminated surface or object - and then touching the eyes, nose, or mouth.
If you stand 1 or 2 meters away from someone with COVID-19, you can be raised through coughing, including when they exhale.
In other words, COVID-19 spreads in a similar way to the flu. Most people infected with COVID-19 experience mild symptoms and recover.
However, some cases of the corona virus continue to experience more serious illness and may require hospitalization.
The risk of disease or infection with the corona virus is increasing for you by the end of 50 and above. This age is said to be more vulnerable than those under 50.
People with weakened immune systems and people with conditions such as diabetes, heart and lung disease are also more susceptible to the corona virus.
d. prevention of corona virus outbreaks If you are sick, reduce contact with others by:
staying at home and self-isolating (unless directed to seek medical care)
if you must leave your home, wear a mask or cover your mouth and nose with tissues, and maintain a 2-metre distance from others
avoiding individuals in hospitals and long-term care centres, especially older adults and those with chronic conditions or compromised immune systems
avoiding having visitors to your home
covering your mouth and nose with your arm when coughing and sneezing
having supplies delivered to your home instead of running errands
supplies should be dropped off outside to ensure a 2-metre distance
It is important to know how you can prepare in case you or a family member become ill.
e. How to handle it
1. Form a core team
The personnel can be taken from the Ministry, State Institutions (K / L) who have a strong social media team such as the Ministry of Education and Culture, Ministry of Communication and Information, BNPB, KPU, TNI, POLRI and elements of community organizations such as NU, MUhammadiyah, and others.
Recruit supervisors from senior journalists with high flying hours and those who are experienced in handling bird flu cases. Gather the person in charge, admin, spokesman or manager of social media in all K / L. Explain the guidelines for handling corona viruses on the internet, websites and social media.
2. Announce a special account
Announce a special account that focuses on conveying information and developments about COVID-19. Until now the public is confused, many Ministry accounts, State Institutions submit information about the corona virus, but mixed with other information.
Accounts do not need to be made new, but can use old accounts with high follower counts. This account refers to a special website that is the center of information.
3. Use a centralized pattern
Using a centralized pattern means that the content is produced by only one team, while the other teams are quite disseminating. It is okay for each K / L to create its own content, but still include sources from the core team. But why make the same content? Better to share, retweet, repost, and others.
Right now, in my observation, what is happening is a pattern of multiple hubs and spoke that is even more severe organic-holistic. That is, every K / L produces content about corona, even many officials or those who are not in office also produce content about it. As a result, the public is increasingly confused because the public relations with certain figures are very strong.
4. Center on Facebook
Why Facebook? Because the interaction column is good for comments and answers. The team can work 7 days 24 hours. Answer all community questions, make Q and A. Give a link that leads to the landing page on each answer.
5. Focus on key messages
Don't use any emoticons or emojis in conveying information and responding to netizens. All communication and information must be based on facts, not emotions and feelings. It should also be remembered that the delivery of information does not create panic, but rather contains technical instructions for prevention.
Build the spirit of fighting for national interests and solidarity, not the ego of the Ministry or the interests of certain groups.
6. Call all social media companies
Call all social media companies operating in Indonesia such as Google, Facebook, YouTube, Instagram, WhatsApp, Twitter, TikTok, LinkedIn, including local social media applications. Ask them to help maximally by referring to the SOP that the government has made.
7. Empower various organizations formed by the government
Organizations such as the Indonesian Enchantment Generation (GENPI) formed by the Ministry of Tourism, for example, can be empowered to help this. According to Kemenpar, GENPI has 15 thousand members spread across 34 provinces and consists of creative young people.
5. After studying and investigating "Corona Virus Handling Protocol" from alternative material or other sources :
a. Design simple information media about the stages of implementing the Corona virus handling protocol in written media. (Done in Separate Sheet).
b. How to respond wisely when there is stigma in the community about the corona virus?
Discrimination should never be allowed
Stigma stops us from moving forward
Fight the virus, not the people
Discrimination is not justified. Be kind
Let’s love and respect people who are working hard in tough times.
6. After the material on Healthy Living, design simple information media about how to implement a healthy way of life. (Done on a separate sheet). Information media material includes:
a. Maintain personal hygiene b. Keep the environment clean c. How to maintain healthy life d. Safe and healthy exercises
7. After observing and learning about the Corona virus and the spread of information in various media that is not necessarily clear or true. If you are a Covid-19 Information Agent, explain how to socialize wisely in the community so that the actions and information conveyed when socializing helps to prevent the spread of disease outbreaks caused by the Corona virus.
be wise in socializing what is done and how to convey the prevention of this corona virus by utilizing existing social media. because we are in a period of isolation which means we have to stay at home to avoid corona virus, then with social media we can convey the prevention of corona virus, through istagram, line, facebook, watsapp, youtube (making vlogs) and others. besides that we are also with us staying at home we can socialize with others through this sophisticated technology media. for example we can phone and video calls, activities online, playing games online, discussing corona viruses online, and utilizing social media.




Komentar
Posting Komentar